Understanding Tailbone Pain: A Common But Ignored Issue
Tailbone pain, also known as coccyx pain or coccydynia, is a discomfort many people silently endure. The tail bones, located at the very bottom of the spine, may be small, but they play a crucial role in providing balance and support when you sit. When these tail bones become injured or inflamed, it can result in persistent tailbone pain that interferes with daily activities.
What Causes Tailbone Pain?
There are several reasons why tailbone pain can occur. Some common causes include:
- Injury or trauma: A fall or direct blow to the tail bones.
- Prolonged sitting: Especially on hard surfaces, which puts pressure on the tail bones.
- Childbirth: A common cause in women due to the pressure exerted on the tail bones.
- Degenerative diseases: Arthritis or bone spurs affecting the tail bones.
- Poor posture: Slouching while sitting can misalign the spine and stress the tail bones.
If left untreated, tailbone pain can become chronic. That’s why early attention and proper care are key to finding a tailbone pain cure.
Tailbone Pain Relief: Home Remedies and Tips
Finding tailbone pain relief doesn’t always mean surgery or strong medication. There are several effective home remedies and lifestyle changes that can help:
1. Use a Cushion
A doughnut-shaped or wedge cushion can take pressure off the tail bones and help ease tailbone pain while sitting.
2. Warm and Cold Compress
Apply an ice pack during the first few days of pain, followed by heat therapy later. This can speed up healing and offer quick tailbone pain relief.
3. Correct Your Posture
Good sitting posture can significantly reduce strain on your tail bones. Sit upright, avoid leaning backward, and keep your feet flat on the floor.
4. Stretch and Exercise
Gentle stretching and pelvic exercises can ease tension around the tail bones and help with a long-term tailbone pain cure.
5. Over-the-Counter Pain Relief
Anti-inflammatory medications can be useful for short-term tailbone pain relief, but they should not be relied on long-term.
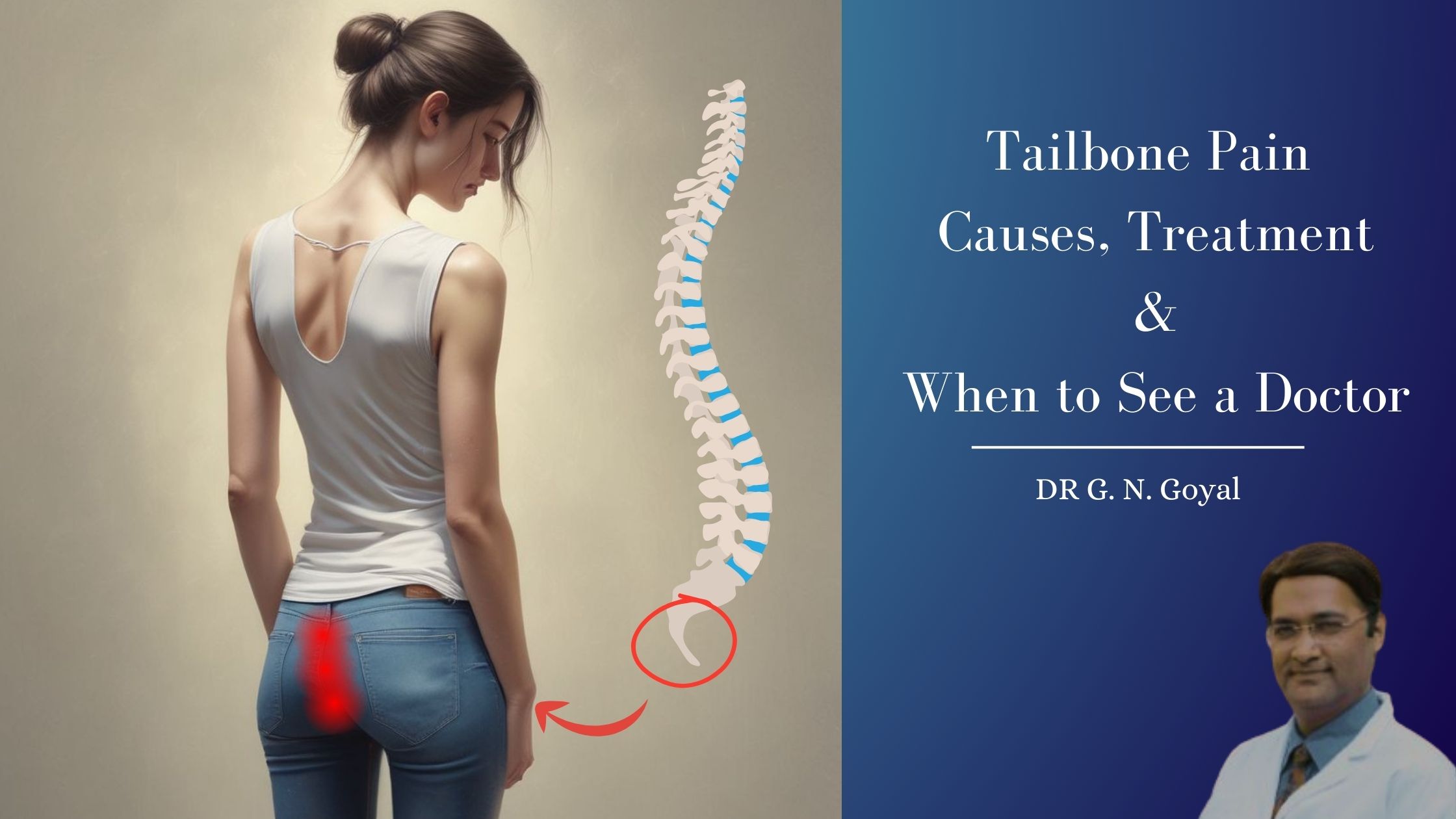
When to Seek Medical Help
If your tailbone pain lasts more than a few weeks, worsens over time, or comes with numbness or tingling, it’s time to consult a healthcare provider, preferable a specialist doctor. They might recommend:
- Physical therapy focused on the lower back and tail bones
- Prescription medications
- MIPSI treatments – Non-surgical, minimally-invasive, keyhole treatments – One of the best treatments available for tailbone pain, offered by Pain Specialist (Spine & Pain Specialist) doctor.
- In rare cases, surgery (coccygectomy) as a tailbone pain cure
Natural Tailbone Pain Cure Options
Many people look for a tailbone pain cure that’s natural and free from side effects. Here are a few suggestions:
- Yoga: Certain yoga poses strengthen and stretch the lower spine and pelvic muscles.
- Salt Baths: Soaking in a warm bath with Epsom salt can ease muscle tension and provide tailbone pain relief.
- Massage Therapy: Deep tissue massage around the lower spine can improve blood flow and reduce pain in the tail bones.
Tailbone pain might feel like a small issue, but it can greatly affect your comfort and quality of life. By understanding the causes and using simple remedies for tailbone pain relief, you can prevent it from becoming a long-term issue. Whether you’re looking for a quick fix or a long-term tailbone pain cure, taking care of your tail bones through posture, cushions, exercises, and therapy can make all the difference.
If the pain continues, don’t hesitate to consult a specialist for personalized tailbone pain relief solutions. Your tail bones deserve just as much attention as any other part of your body!
Do you suffer from tailbone pain? Share your experience in the comments below!
Visit the Tailbone Pain Specialist or for any other lower back related Problems in Delhi, Haryana or Punjab Dr. G N Goyal, at the nearest Tailbone Pain Clinic, and book your appointment now!
CONTACT US
You may please click here, to know the pleasant experiences of our patients.